Introduction
In the landscape of oral health, jaw cavitations stand as a lesser-known but significant concern. These cavitations, characterized by areas of necrotic bone often found after tooth extractions, can harbor a variety of pathogens and contribute to chronic inflammation. Despite their potential systemic impact, jaw cavitations are frequently undiagnosed due to their asymptomatic nature. In this comprehensive exploration, we delve into the intricacies of jaw cavitations, from their formation and causes to detection, systemic implications, treatment options, and preventive measures.
Understanding Jaw Cavitations
Jaw cavitations, also known as osteonecrosis of the jaw, occur when areas of the jawbone fail to heal properly following tooth extractions, leading to the formation of hollow pockets within the bone (Nanci, 2012). These cavitations can serve as breeding grounds for infections, fostering chronic inflammation that may extend beyond the oral cavity. While initially asymptomatic, jaw cavitations can progress over time, posing significant health risks if left untreated.
Formation and Causes
The development of jaw cavitations is often attributed to factors such as inadequate blood supply, infection, and clotting issues during tooth extraction procedures (Gagliano et al., 2011). Trauma sustained during extraction can compromise the blood vessels in the jawbone, impeding proper blood flow and resulting in bone death. Additionally, the introduction of bacteria into the extraction site can lead to infection and subsequent necrosis. Failure to form a stable blood clot at the extraction site further exacerbates the risk of bone exposure and bacterial infiltration.
Symptoms and Detection
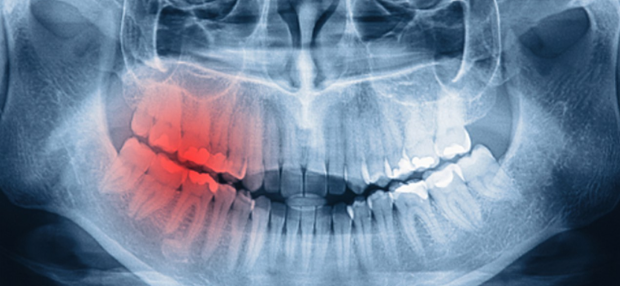
Early-stage jaw cavitations typically manifest without overt symptoms, making them challenging to detect clinically. However, as the condition progresses, individuals may experience chronic pain, swelling, or sinus issues near the affected area. Diagnostic imaging, particularly 3D cone beam radiography, is instrumental in identifying jaw cavitations, providing detailed insights into bone health and revealing necrotic areas that may not be apparent on conventional dental x-rays (Scarano et al., 2010).
Systemic Implications
Beyond their local effects within the oral cavity, jaw cavitations can have far-reaching systemic implications. The pathogens harbored within these cavitations can trigger chronic inflammation, leading to immune system dysfunction and contributing to the development or exacerbation of various chronic diseases (Marx, 2003). Moreover, bacteria from cavitations can enter the bloodstream, potentially seeding infections in distant sites or inciting systemic inflammatory responses.
Treatment Options

Effective management of jaw cavitations often necessitates surgical intervention to remove necrotic bone tissue and eliminate infection. Debridement procedures aim to thoroughly clean the affected area, facilitating optimal healing and bone regeneration. Post-surgery, supportive therapies such as ozone therapy, nutritional supplementation, and regenerative treatments like platelet-rich plasma therapy can aid in recovery and reduce the risk of recurrence (Ruggiero et al., 2009).
Prevention
Preventing jaw cavitations requires a multifaceted approach encompassing careful dental procedures, regular dental check-ups, and optimal oral hygiene practices. By prioritizing patient safety during tooth extractions, monitoring oral health status, and promoting good oral hygiene habits, dental professionals can mitigate the risk of cavitation formation and promote overall oral health.
The Impact of Oral Microbiome
An essential aspect contributing to the pathogenesis of jaw cavitations is the oral microbiome. The human oral cavity harbors a diverse array of microorganisms, including bacteria, fungi, and viruses, collectively known as the oral microbiome. Under normal circumstances, these microorganisms maintain a delicate balance, contributing to oral health and homeostasis. However, disruptions to this microbial equilibrium, such as those occurring during tooth extractions or due to poor oral hygiene, can pave the way for dysbiosis—a state characterized by microbial imbalance and dysregulated immune responses (Jiao et al., 2014).
The Role of Inflammation
Chronic inflammation lies at the heart of jaw cavitations, driving the pathogenesis and perpetuation of these silent lesions. In response to microbial invasion and tissue injury, the immune system initiates an inflammatory cascade, mobilizing immune cells and releasing pro-inflammatory mediators. While acute inflammation serves as a protective response, chronic inflammation in the context of jaw cavitations can have deleterious effects, leading to tissue damage, bone resorption, and systemic immune dysregulation (Graves et al., 2012).
Diagnostics Advancements
Recent advancements in diagnostic imaging have revolutionized the detection and characterization of jaw cavitations. Techniques such as 3D cone beam computed tomography (CBCT) provide high-resolution, three-dimensional images of the maxillofacial region, enabling precise visualization of bone anatomy and pathology (Pauwels et al., 2012). By offering unparalleled insights into the structural integrity of the jawbone and identifying subtle abnormalities indicative of cavitation formation, CBCT has emerged as a cornerstone in the diagnosis and treatment planning of jaw cavitations.
Nutritional Considerations
Nutritional status plays a crucial role in the prevention and management of jaw cavitations. Adequate intake of essential nutrients, including vitamins D and K, calcium, magnesium, and antioxidants, supports bone health and immune function, fostering optimal healing and tissue regeneration post-surgery (Cockayne et al., 2006). Conversely, deficiencies in key micronutrients can compromise the body’s ability to repair damaged tissues and mount an effective immune response, potentially prolonging recovery time and increasing susceptibility to infection.
Patient Education and Empowerment
Empowering patients with knowledge about jaw cavitations and preventive measures is paramount in mitigating the risks associated with these silent lesions. Dental professionals play a pivotal role in educating patients about the importance of maintaining optimal oral hygiene, attending regular dental check-ups, and adopting healthy lifestyle habits conducive to overall oral and systemic health (Coulter et al., 2015). By fostering open communication and collaborative decision-making, dental providers can empower patients to take proactive steps in preserving their oral health and well-being.
Conclusion
Jaw cavitations represent a significant yet often overlooked threat to oral and systemic health. By raising awareness of their causes, risks, and treatment options, both patients and dental professionals can work collaboratively to address this silent menace. Early detection, prompt intervention, and preventive measures are essential in mitigating the impact of jaw cavitations and safeguarding oral and overall well-being for all individuals.