Introduction
Biotransformation, commonly referred to as detoxification, is a crucial biological process within the human body that plays a vital role in removing both externally acquired and internally generated toxins. This process is essential for maintaining overall health and involves the biochemical conversion of fat-soluble toxins into water-soluble forms, which the body can then safely excrete. Operating continuously and unobtrusively, biotransformation ensures that our elimination pathways function efficiently, safeguarding us from potential toxin buildup which could otherwise lead to health issues.
Detailed Breakdown of the Biotransformation Phases
Biotransformation consists of three distinct phases, each critical to the effective elimination of toxins:
- Phase I (Transformation): This phase occurs primarily in the liver, involving enzymes mainly from the cytochromes P450 family, which modify toxins through oxidation, reduction, and hydrolysis. This modification makes the toxins slightly less harmful and prepares them for further processing. The cytochromes P450 are responsible for the biotransformation of approximately 75% of total drugs in clinical use, indicating their crucial role in detoxification (Guengerich, 2008).
- Phase II (Conjugation): Also taking place in the liver, this phase involves the conjugation of the modified toxins from Phase I with other substances to increase their water solubility. Typical conjugation reactions include glucuronidation, sulfation, and conjugation with amino acids like glutathione. Glutathione conjugation, for instance, plays a pivotal role in detoxifying endogenous compounds and xenobiotics (Lushchak, 2012).
- Phase III (Excretion): This final phase happens in the kidneys and digestive system, where the now water-soluble toxins are prepared for elimination from the body through urine or feces. It is crucial for the actual removal of toxins from the body.
Each of these phases is vital not only for detoxification but also for maintaining overall health. However, they also generate free radicals as byproducts, which can lead to oxidative stress if not adequately neutralized by antioxidants. This oxidative stress can impair mitochondrial structure and function, highlighting the need for specific nutritional support during detoxification.
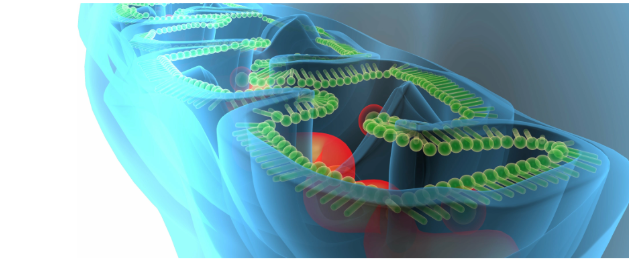
The Central Role of Mitochondria in Energy and Detoxification
Mitochondria are subcellular structures that generate most of the cell’s supply of adenosine triphosphate (ATP), used as a source of chemical energy. In the context of biotransformation, mitochondria are absolutely critical because they supply the energy required for the detox processes. The liver and kidneys, which are heavily involved in detoxification, are also rich in mitochondria. The liver, for instance, not only performs complex biochemical transformations but also requires a significant amount of energy—about 18% of the body’s daily energy expenditure. Each liver cell contains approximately 1,000 to 2,000 mitochondria (Wallace, 2012). Similarly, the kidneys use about 10% of the body’s total daily energy expenditure, relying heavily on mitochondrial function for nutrient reabsorption and metabolic activities, including filtering waste (Smith et al., 2013).
Gastrointestinal Health and Its Impact on Detoxification

The health of the gastrointestinal tract is fundamental to the effective third phase of biotransformation. Any disruption in gastrointestinal health, such as dysbiosis or constipation, can impede the removal of toxins, complicating the detox process. Dietary choices play a significant role in maintaining gut health; for example, a diet low in fiber and high in sugars and processed foods can detrimentally affect gastrointestinal function and, by extension, biotransformation.
Furthermore, the alarming statistic that 95% of Americans are deficient in at least one essential nutrient underscores the necessity of a nutrient-rich diet. Adequate levels of fiber and essential micronutrients are crucial for supporting the digestive processes and, consequently, the entire detoxification pathway (CDC, 2017).
The Paradox of Biotransformation and Mitochondrial Function
A complex challenge within biotransformation is the need for ATP to effectively clear toxins, which, paradoxically, can impair mitochondrial ATP production. The continuous rise in environmental toxins contributes to an increased toxic burden, potentially overwhelming the body’s detox capabilities and impacting mitochondrial function. This can manifest in symptoms such as fatigue, brain fog, hormonal imbalances, and unexplained weight gain, indicating a compromised detoxification process.
Empowering Patients Through Comprehensive Detoxification Support
Empowering patients in their health journeys involves not only educating them about the processes and challenges of biotransformation but also providing them with tools and strategies to enhance their detoxification capacity. This includes nutritional support to bolster mitochondrial function, lifestyle changes to reduce toxin exposure, and dietary adjustments to improve gastrointestinal health. By addressing these areas, healthcare providers can significantly enhance their patients’ ability to manage and eliminate toxins, leading to better health outcomes.
Conclusion
Understanding and supporting biotransformation processes are crucial for maintaining health and preventing disease. Through comprehensive detox strategies that include dietary optimization, lifestyle adjustments, and regular health check-ups, individuals can enhance their body’s natural detoxification capabilities and achieve better long-term health outcomes.